Connecticut legislators have lofty ambitions to tackle major health and human services challenges during the 2026 legislative session, which begins on Feb. 4 and runs through May 6.
Legislators will take another crack at addressing two key health care issues that have come up repeatedly in the past several years but failed to see substantial progress: increasing Medicaid reimbursement to providers and passing legislation to rein in private equity investment in health care.
Meanwhile, the Committee on Children will be focused on oversight and budgetary concerns at the Department of Children and Families — a direct response to recent tragic deaths of children, including the starvation of Jacqueline “Mimi” Torres-García whose body was discovered in New Britain in October 2025.
Medicaid reimbursement rates
Legislators will make another push for at least the fourth year in a row to meaningfully increase how much the state pays medical providers to treat patients with Medicaid coverage.
“We put money into the budget last year,” Human Services Committee co-Chair Rep. Jillian Gilchrest, D-West Hartford, said. “But it wasn’t nearly what’s needed.”
Last year’s budget allocated $60 million over fiscal years 2026 and 2027 to boost rates for most providers, which fell far short of a proposal led by the Human Services Committee to increase spending by more than $250 million by 2028-29.
For years, physicians and legislators have been sounding the alarm that prevailing Medicaid reimbursement rates are too low, making it unaffordable for health care providers to treat patients with Medicaid coverage, thus decreasing access to care for those residents.
Sen. Jason Perillo, R-Shelton, a ranking member on the Human Services Committee, said the low reimbursement rates also impact the business community by shifting cost of care to commercial insurers, which drives up premiums for employers and employees.
“Anything we can do to increase reimbursements to hospitals and other providers will go a long way to make Connecticut a more business-friendly state,” Perillo said.
Despite bipartisan support, Gov. Ned Lamont has been reluctant to fund broad reimbursement increases.
Last year, he proposed spending $35.4 million to boost rates over the biennium, much lower than the Human Services Committee’s proposal and also less than a House Republican proposal to spend $138 million over the same time period. However, the House GOP plan pitched eliminating Medicaid coverage for undocumented residents to help pay for the Medicaid rate boost.
Private equity
Regulating private equity investment in health care is another area where years of proposals have failed, despite broad consensus that something needs to be done.
In 2024, legislators considered, but ultimately failed to pass, a handful of bills aimed at reining in private equity following highly publicized financial struggles at three Connecticut hospitals owned by Prospect Medical Holdings, a formerly private equity-backed national health system. In January of last year, Prospect filed for bankruptcy, once again reigniting calls to rid the state’s health systems of private equity.
The governor proposed increasing oversight of major health care industry transactions — such as hospital mergers and acquisitions — by broadening the types of deals that would require state review to include those typically used by private equity-backed operators. A bill put forth by the Public Health Committee focused on banning private equity involvement outright in certain parts of the health care system.
But the two sides failed to come together on a single proposal before the end of session.
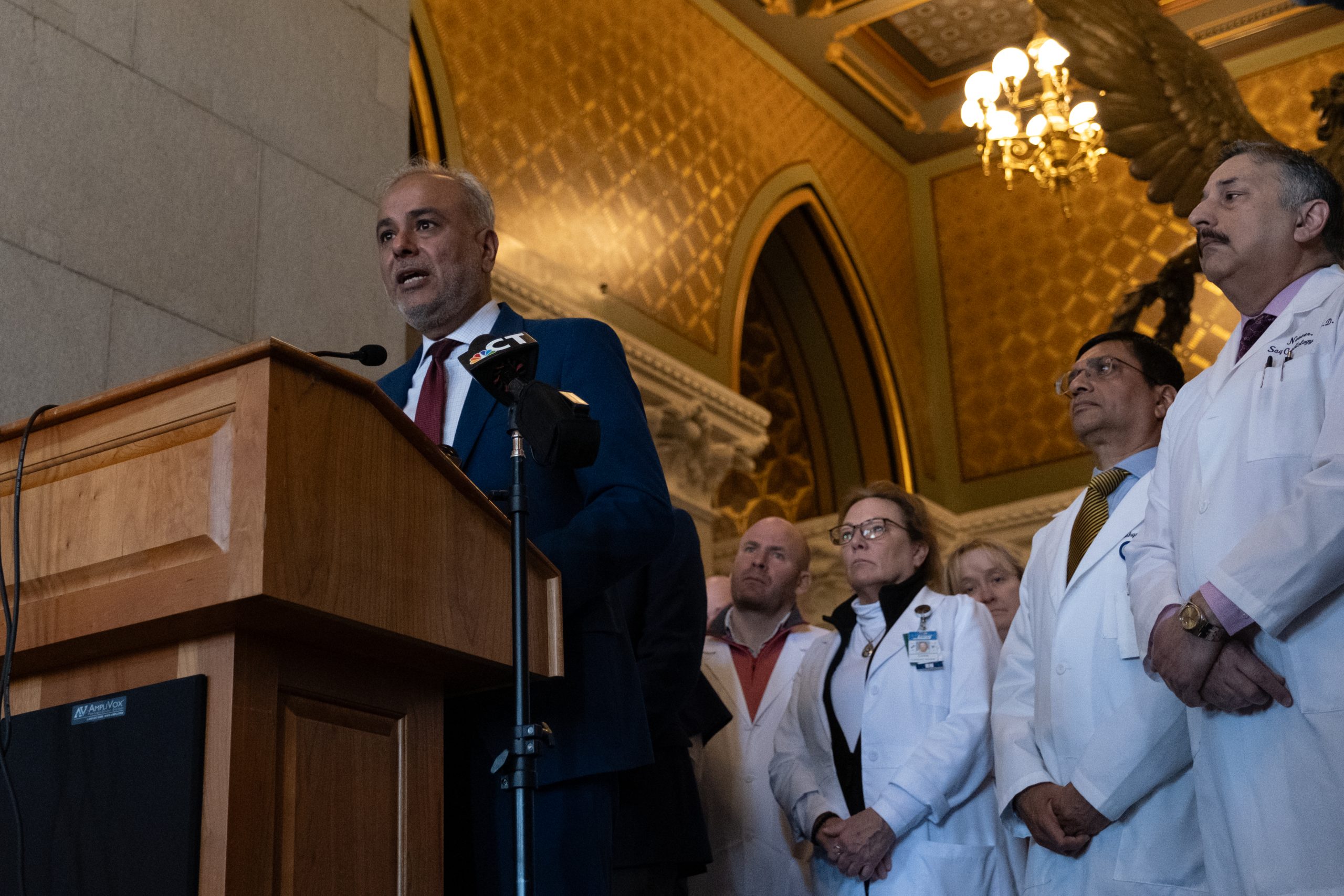
Public Health Committee co-chair and practicing physician Saud Anwar, D-South Windsor, said he garnered buy-in from hospitals and physician groups on a measure to prohibit private equity investment in hospitals specifically. That will be the starting point for this year’s proposals.
Sen. Jeff Gordon, R-Woodstock, also a practicing physician who has been active on the issue of private equity, agreed with the approach, saying the state should “ban private equity from having any financial interest whatsoever in hospitals or severely [regulate] them so they never want to come back to Connecticut and be involved with hospitals.”
DCF oversight
Rep. Corey Paris, D-Stamford, who co-chairs the Committee on Children, said that this year’s effort to reform DCF will be guided by a simple principle: “When a state steps into a child’s life, we must get it right, and that means accountability, transparency and making sure that families are supported before crises becomes tragedies,” Paris said.
Paris’s co-chair, Sen. Ceci Maher, D-Wilton, agreed. She sees the death of 11-year-old Torres-García last October as the driving force behind a renewed effort to scrutinize the agency and see whether additional funds are needed to better support its employees and operations.
“We want to work with DCF to make certain that never happens again,” Maher said. “We are very aware that there needs to be a deep-dive looking at DCF — their needs, staffing, funding, to make sure that we are supporting them, but also making sure that our children are safe.”
Maher said she plans to propose legislation that would prevent someone who has served time for abusing a child from living in a home with children after their incarceration. Jackelyn García, the aunt of Torres-García who has been charged for crimes in connection with her murder, was previously convicted of abusing a child and served time in York Correctional Institution, according to an arrest warrant.
The Committee on Children will also be looking to restart a discussion on regulating municipal camps that gained momentum in 2025 after a child abuse case in Bethany brought attention to the lack of required background checks or other regulations for staff who work at town-run programs for children.
Response to federal policy changes — vaccines, funding
The past year has brought seismic shifts in federal health policy that will impact the state budget, including pending changes to Medicaid eligibility and the expiration of enhanced premium tax credits for Affordable Care Act, or ACA, plans.
The Lamont administration has already responded to some of these changes directly. Last month, the governor announced a one-time investment of $115 million in state funds to help offset the expiring federal tax credits for some of the residents that will be hardest hit by the policy change.
Sen. Matt Lesser, D-Middletown, who co-chairs the Human Services Committee, said he would like to see additional funding go toward people who may not qualify for the initial state subsidies, and also look at policies to sustain state support going forward.
“Figuring out what we can do to address the affordability of health insurance is really my top focus,” Lesser said.
Sen. Jorge Cabrera, D-Hamden, who co-chairs the Insurance Committee, agreed.
“Health care is the issue for the state and the country. I’m glad our committee is in a position to do something about it,” Cabrera said.
But exactly how to achieve that expanded coverage is still in discussion, though Lesser suggested the creation of a Connecticut Health Care Trust Fund to “fund ongoing subsidies or other supports to bring down the cost of private health insurance.”
Lesser also said he’d like to see the legislature address coming increases in uncompensated care to hospitals and food insecurity resulting from new SNAP work requirements.
Public Health Committee co-chairs Anwar and Rep. Cristin McCarthy Vahey said there will also be an effort, led by the governor’s office and the Department of Public Health, to give Connecticut more authority over vaccine recommendations and purchases.
McCarthy Vahey said the goal is to “maintain best practices” around vaccinations.
A draft proposal includes measures to extend the DPH commissioner’s authority to recommend vaccines for adults and give the agency’s vaccine program the power to purchase all child and adult vaccines needed to meet the state’s recommendations.
DPH Commissioner Manisha Juthani already has exercised some power in this area. Juthani issued guidance on COVID-19 vaccines and childhood vaccines that maintained recommendations previously in place, despite changes from the federal government.